How Gut Health Impacts Pelvic Floor Function and Overall Wellness
How Gut Health Impacts Pelvic Floor Function and Overall Wellness
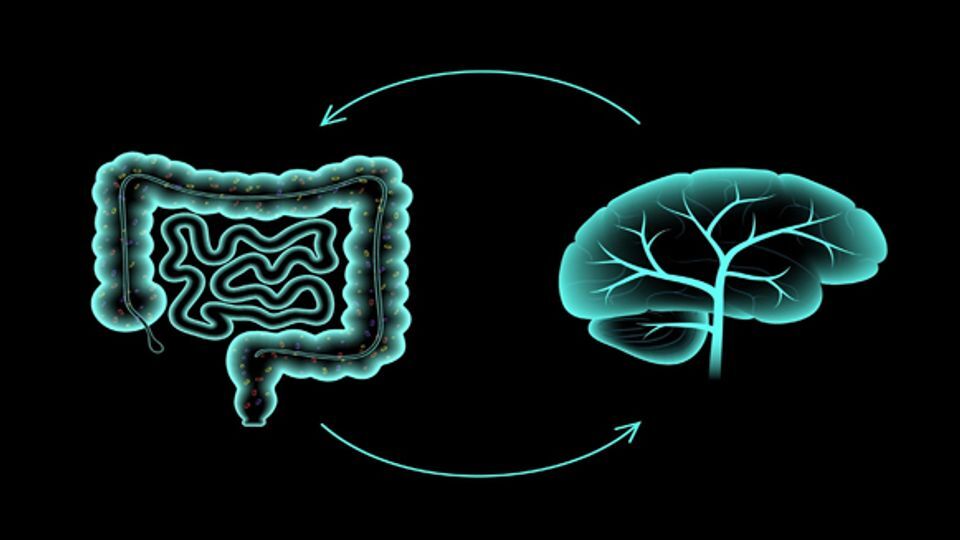
The human body is a complex, interconnected system, with many processes influencing each other. One of the most fascinating connections is the relationship between the gut and the brain—a connection often referred to as the gut-brain axis. This bidirectional communication pathway between the gastrointestinal (GI) system and the central nervous system (CNS) has profound implications not only for digestive health but also for pelvic health.
In this blog post, we’ll explore what the gut-brain axis is, how it impacts pelvic health, and how a dysregulated gut-brain connection can contribute to issues like pelvic pain, constipation, incontinence, and more. We will also discuss strategies for improving the gut-brain relationship to optimize pelvic health.
What is the Gut-Brain Axis?
The gut-brain axis refers to the communication network that links the gut and the brain. This relationship is facilitated through multiple channels, including:
The Vagus Nerve: The vagus nerve is the longest cranial nerve and acts as a primary conduit for communication between the gut and the brain. It helps regulate a variety of autonomic functions, including digestion, heart rate, and breathing.
The Enteric Nervous System (ENS): Often called the "second brain," the ENS is a complex network of neurons embedded in the walls of the gastrointestinal tract. The ENS can operate independently of the brain and spinal cord, but it is still heavily influenced by signals from the brain.
Neurotransmitters and Hormones: The gut produces a wide variety of neurotransmitters, such as serotonin, dopamine, and GABA, that not only regulate gut function but also influence mood, stress levels, and cognitive function. About 90% of the body’s serotonin is found in the gut, suggesting a strong link between gut health and mental health.
Immune System Signals: The gut is home to a large portion of the body’s immune cells. The immune response in the gut can affect inflammation levels throughout the body, including the pelvic area.
This intricate connection means that the gut and brain are in constant communication, sending and receiving signals that affect each other's function. When this communication becomes disrupted, it can lead to a range of physical and mental health problems, including those affecting the pelvic region.
How the Gut-Brain Axis Affects Pelvic Health
The health of your gut can have far-reaching effects on pelvic health. Below are several ways in which the gut-brain axis plays a crucial role in the function of the pelvic floor and the surrounding structures:
1. Chronic Pelvic Pain and Sensitization
Pelvic pain is a common issue, and in many cases, it can be linked to an underlying disruption in the gut-brain axis. The brain’s perception of pain is influenced by sensory information coming from both the gut and the pelvic floor.
- Visceral hypersensitivity: A disrupted gut-brain connection can increase sensitivity to pain signals, resulting in heightened pain perception, even from stimuli that would normally be non-painful. This phenomenon is referred to as visceral hypersensitivity and can affect both the gastrointestinal system and the pelvic organs.
- Pelvic pain syndromes: Conditions like interstitial cystitis, vulvodynia, and endometriosis are often associated with a dysregulated gut-brain axis. The brain may overreact to normal pelvic sensations, causing chronic pain and discomfort.
2. Constipation and Pelvic Floor Dysfunction
The health of the gut is deeply intertwined with the function of the pelvic floor. Chronic constipation and straining during bowel movements can lead to pelvic floor dysfunction over time.
- When constipation becomes a chronic issue, the pelvic floor muscles can become overactive and tight, leading to difficulty in relaxing the muscles for proper bowel movements. In turn, this increases intra-abdominal pressure, which can contribute to issues like pelvic organ prolapse or urinary incontinence.
- A dysfunctional gut-brain connection may contribute to constipation by affecting the enteric nervous system, which regulates bowel motility and coordination. Stress, anxiety, and other emotional factors can exacerbate constipation through their influence on the gut-brain communication.
3. Irritable Bowel Syndrome (IBS) and Pelvic Health
Irritable Bowel Syndrome (IBS) is a condition that affects many people with pelvic floor dysfunction. The relationship between IBS and pelvic health is well-documented, as both conditions share common mechanisms in the gut-brain axis.
- IBS is a functional disorder of the gut characterized by symptoms like bloating, gas, diarrhea, and constipation. Stress and anxiety can trigger or worsen IBS symptoms, and in turn, gut inflammation or altered motility can exacerbate pelvic floor dysfunction. Many individuals with IBS also experience pelvic discomfort or pain, making the link between gut and pelvic health particularly important.
4. Urinary Incontinence and the Gut-Brain Axis
Urinary incontinence can be exacerbated by the gut-brain connection, especially when there is an underlying issue with constipation or IBS. For instance:
- Straining and increased intra-abdominal pressure caused by chronic constipation can affect the bladder and contribute to stress urinary incontinence (SUI).
- Additionally, the brain’s perception of bladder signals can be altered by the gut-brain axis. An overactive bladder or bladder urgency may be linked to digestive issues and dysregulated communication between the gut and brain.
Improving the Gut-Brain Connection for Pelvic Health
While the gut-brain axis is complex, there are several strategies that can help improve its function and, by extension, benefit pelvic health:
1. Mindful Eating and Gut Health
Eating a balanced diet rich in fiber, prebiotics, and probiotics can support gut health and improve the functioning of the gut-brain axis. Fiber-rich foods support bowel regularity, while probiotics help maintain a healthy gut microbiome, which influences gut-brain communication.
- Fermented foods like yogurt, kefir, and kimchi, as well as prebiotic foods like garlic, onions, and bananas, can enhance gut health and reduce inflammation, which may alleviate symptoms of pelvic floor dysfunction.
2. Managing Stress
Since stress has a direct impact on the gut-brain connection, it’s important to incorporate stress management techniques into your daily routine. Mindfulness practices, meditation, yoga, and deep breathing can help reduce the negative effects of stress on the gut and improve pelvic floor function.
- Breathing exercises and relaxation techniques can help regulate the autonomic nervous system, which in turn reduces gut and pelvic floor tension.
3. Pelvic Floor Exercises and Relaxation
For those experiencing pelvic floor dysfunction as a result of gut issues, incorporating both pelvic floor strengthening and relaxation techniques can be beneficial.
- Pelvic floor relaxation exercises, such as deep breathing and diaphragmatic breathing, can help reduce the tension in the pelvic floor muscles that may result from chronic constipation or stress.
- Pelvic floor strengthening exercises like Kegels can help improve pelvic muscle tone, especially when constipation or IBS leads to weakness or incoordination of these muscles.
4. Professional Support
If you’re experiencing persistent pelvic or gastrointestinal issues, it’s important to seek professional help. A pelvic floor physiotherapist can work with you to address any muscle dysfunction and provide exercises tailored to your specific needs. Additionally, consulting with a gastroenterologist or dietitian can help identify any underlying gut issues contributing to pelvic health concerns.
Conclusion
The gut-brain axis is a fascinating and essential part of human physiology, with profound effects on pelvic health. A dysregulated connection between the gut and the brain can contribute to pelvic pain, incontinence, constipation, and more. By understanding how gut health impacts pelvic floor function and implementing strategies to improve gut-brain communication, individuals can better manage pelvic health concerns.
If you’re dealing with pelvic health issues, improving your gut health through mindful eating, stress management, and pelvic floor exercises can make a significant difference in your overall well-being. Don’t hesitate to reach out to healthcare professionals who can help guide you through this complex relationship and create a treatment plan tailored to your needs.