How the Brain and Nerves Control Your Bladder.
Introduction
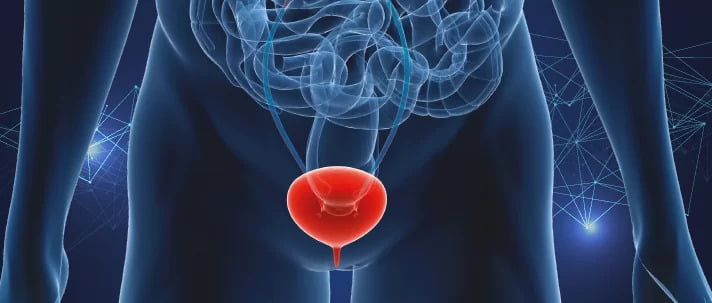
The bladder is a vital organ responsible for storing and releasing urine. Its complex functioning relies on a sophisticated network of nerves and muscles. In this article, we will explore the intricate mechanisms involved in bladder function, including the neural connections, control from the brain and peripheral nerves, and the role of bladder muscles.
I. Anatomy of the Bladder:
The bladder is a hollow, muscular organ located in the pelvis. It is composed of several layers, including the inner lining called the urothelium, the muscular layer known as the detrusor muscle, and surrounding connective tissue.
II. Neural Control of the Bladder:
- Autonomic Nervous System (ANS): The bladder's neural control primarily involves the autonomic nervous system, which consists of two branches: the sympathetic and parasympathetic nervous systems.
- Sympathetic Nervous System: The sympathetic nerves innervating the bladder originate from the lower thoracic and upper lumbar spinal cord. Activation of the sympathetic nerves inhibits bladder contraction, promoting urine retention.
- Parasympathetic Nervous System: The parasympathetic nerves originate from the sacral spinal cord (S2-S4) and are responsible for bladder contraction. Stimulation of the parasympathetic nerves triggers the micturition reflex, leading to bladder emptying.
III. Micturition Reflex:
- Micturition Center: The micturition center is located in the sacral spinal cord and receives sensory input from the bladder through the pelvic nerves. It integrates signals from the bladder, brain, and spinal cord to coordinate bladder contractions and control the timing of urination.
- Sensory Pathways: Sensory information from the bladder is transmitted to the micturition center via afferent nerves. These nerves sense bladder filling, stretch, and pressure, signaling the need for voiding.
- Motor Pathways: Once the bladder reaches a certain threshold of distension, the micturition center sends signals via efferent nerves to initiate bladder contraction. The detrusor muscle contracts while the bladder neck and urethral sphincters relax, facilitating urine flow.
IV. Control from the Brain:
- Higher Brain Centers: The cerebral cortex and brainstem play important roles in controlling bladder function. The frontal cortex, prefrontal cortex, and limbic system influence voluntary control and decision-making regarding urination.
- Descending Pathways: These neural pathways from the brainstem and cortex modulate the micturition reflex. They can facilitate or inhibit the reflex, allowing conscious control over bladder function.
V. Bladder Muscles:
- Detrusor Muscle: The detrusor muscle is the main muscle of the bladder wall responsible for contracting and expelling urine. It consists of smooth muscle fibers that contract during the micturition reflex under parasympathetic stimulation.
- External Urethral Sphincter: The external urethral sphincter is a voluntary muscle located at the junction of the bladder and urethra. It remains contracted during urine storage, maintaining urinary continence. During micturition, it relaxes under conscious control to allow urine to flow.
VI. Disorders and Dysfunctions:
- Overactive Bladder: Overactive bladder is characterized by sudden and frequent urges to urinate due to involuntary bladder contractions. It can result from an overactive detrusor muscle or abnormal neural signaling.
- Urinary Incontinence: Urinary incontinence refers to the involuntary leakage of urine. It can be caused by weakened pelvic floor muscles, impaired bladder control, or neurological conditions affecting bladder function.
- Neurogenic Bladder: Neurogenic bladder occurs when there is a disruption in the normal neural control of the bladder. It can result from conditions such as spinal cord injury, multiple sclerosis, or diabetic neuropathy, leading to difficulties in bladder emptying or urine retention.
- Urinary Retention: Urinary retention refers to the inability to fully empty the bladder. It can be caused by weakened bladder muscles, obstruction in the urinary tract, or nerve damage affecting bladder control.
VII. Diagnosis and Treatment:
- Diagnostic Tools: Several diagnostic tests can evaluate bladder function, including urodynamic studies, cystoscopy, and imaging techniques. These tests help identify underlying causes and guide appropriate treatment.
- Treatment Approaches: Treatment for bladder dysfunctions depends on the specific condition but may include lifestyle modifications, pelvic floor exercises, behavioral interventions, medications, and in some cases, surgical interventions.
Conclusion:
The functioning of the bladder is a complex interplay between neural control, muscular coordination, and sensory feedback. Understanding the neural connections and mechanisms involved in bladder function is crucial for diagnosing and managing bladder disorders.
The autonomic nervous system, micturition reflex, and higher brain centers all play integral roles in coordinating bladder contractions and maintaining continence. Disorders such as overactive bladder, urinary incontinence, and neurogenic bladder can significantly impact an individual's quality of life, but with proper diagnosis and treatment, many of these conditions can be effectively managed.
Pelvic physiotherapy, along with other therapeutic interventions, offers a range of techniques to address bladder dysfunctions and promote optimal bladder health. By targeting the underlying causes, strengthening pelvic floor muscles, and improving neural control, pelvic physiotherapy can help restore bladder function and alleviate symptoms.