How Cancer Treatment Can Lead to Pelvic Issues
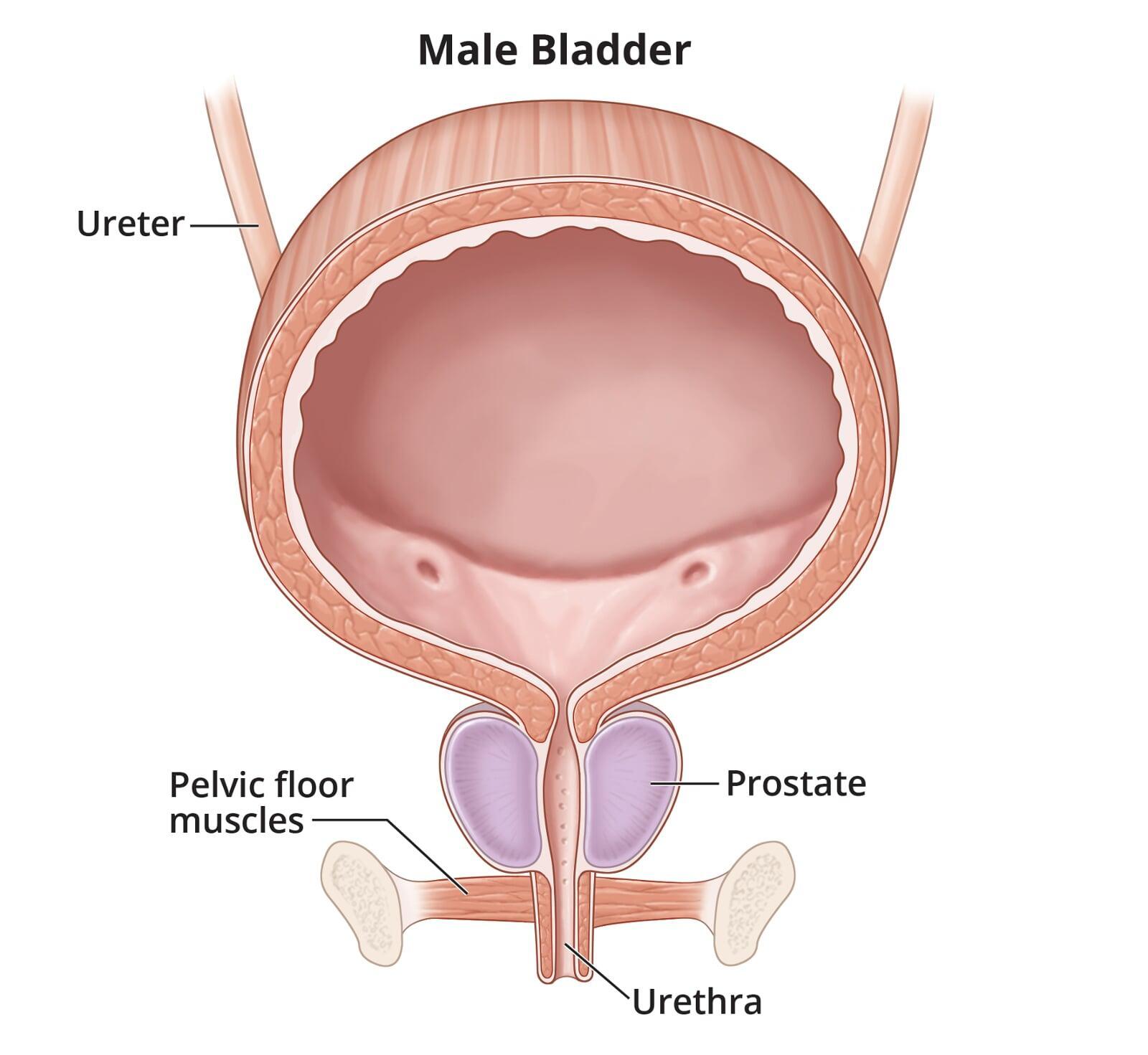
Prostate cancer is one of the most common cancers among men, and advancements in early detection and treatment have greatly improved outcomes. However, prostate cancer treatments—such as surgery, radiation, and hormone therapy—can have a significant impact on pelvic floor health. The pelvic floor, which consists of muscles and connective tissues that support the bladder, bowel, and sexual organs, plays a crucial role in urinary control, sexual function, and overall quality of life. Unfortunately, prostate cancer treatments can affect the pelvic floor, leading to a range of physical and emotional challenges.
This post explores the effects of prostate cancer treatment on pelvic floor health and the role of pelvic floor physiotherapy in addressing these challenges.
Prostate Cancer Treatment Options and Their Impact on the Pelvic Floor
The treatment approach for prostate cancer depends on several factors, including the stage and grade of the cancer, the patient's overall health, and personal preferences. Common treatments include:
- Radical Prostatectomy (Surgical Removal of the Prostate)
- External Beam Radiation Therapy
- Hormone Therapy (Androgen Deprivation Therapy)
- Brachytherapy (Radioactive Seed Implants)
While these treatments can be life-saving, they may also have side effects that impact the pelvic floor muscles and function. Understanding these effects can help patients and healthcare providers make informed decisions about post-treatment care.
1. Radical Prostatectomy (Surgical Removal of the Prostate)
Radical prostatectomy is one of the most common surgical treatments for prostate cancer. During the procedure, the prostate gland is removed, and sometimes surrounding tissues are also taken out. This surgery can result in damage to the nerves and muscles surrounding the prostate, including those of the pelvic floor. The pelvic floor muscles are essential for urinary control, sexual function, and providing stability to the pelvic region.
After surgery, many men experience:
Urinary Incontinence: The prostate and surrounding tissues play a role in controlling urination. Damage to the nerves or muscles involved in bladder control during prostatectomy can result in urinary incontinence (the inability to control urine flow). While this is a common post-surgical side effect, it is often temporary and can be managed with pelvic floor physiotherapy.
Erectile Dysfunction: The pelvic floor muscles also contribute to sexual function, including erectile function and ejaculation. Damage to the nerves or tissues during surgery can cause erectile dysfunction, although recovery is possible with appropriate treatment.
Pelvic Floor Weakness and Imbalance: The surgical removal of the prostate can lead to pelvic floor muscle weakness or imbalance. Weakness in these muscles can further contribute to incontinence and difficulty with sexual function. Pelvic floor rehabilitation is often needed to strengthen the muscles and restore proper function.
2. Radiation Therapy
Radiation therapy, often used when prostate cancer is localized or when surgery is not an option, involves using high-energy radiation to kill cancer cells. While effective at treating cancer, radiation can cause damage to the pelvic floor muscles and surrounding tissues, leading to several potential complications:
Urinary Issues: Similar to prostatectomy, radiation can damage the bladder and urinary sphincters, leading to incontinence, urgency, and frequency. These symptoms may develop gradually over time and may be long-lasting, requiring pelvic floor rehabilitation to improve control and function.
Rectal Dysfunction: Radiation therapy can also affect the muscles of the rectum and anus, leading to issues such as fecal incontinence or difficulty controlling bowel movements. Pelvic floor physiotherapy can help improve control over bowel movements and support the muscles involved in the rectal area.
Sexual Dysfunction: Radiation therapy can damage blood vessels and nerves that are involved in erectile function, leading to erectile dysfunction. Although the treatment might not directly affect the pelvic floor muscles, it can exacerbate issues like sexual dysfunction when combined with other pelvic floor impairments.
3. Hormone Therapy (Androgen Deprivation Therapy)
Hormone therapy, or androgen deprivation therapy (ADT), is often used in conjunction with other treatments for prostate cancer. ADT reduces the levels of testosterone, which can slow the growth of cancer cells. However, this treatment has a number of side effects, some of which directly impact the pelvic floor and sexual health:
Loss of Muscle Mass: One of the side effects of ADT is a reduction in muscle mass and strength, which can affect the pelvic floor muscles. Weakened pelvic floor muscles can contribute to urinary incontinence and sexual dysfunction.
Erectile Dysfunction: Reduced testosterone levels can impair erectile function, and in combination with the effects of prostate cancer treatments, can result in long-term sexual difficulties.
Decreased Bone Density: ADT can reduce bone density, increasing the risk of fractures and affecting the stability of the pelvic region, which in turn can exacerbate pelvic floor dysfunction.
4. Brachytherapy (Radioactive Seed Implants)
Brachytherapy involves the placement of radioactive seeds directly into the prostate to treat cancer. While less invasive than surgery, it can still have some impact on the pelvic floor, although generally to a lesser degree. The most common effects include:
Urinary Issues: Like other treatments, brachytherapy can cause urinary symptoms, including incontinence and frequency, due to damage to the bladder and surrounding tissues.
Pelvic Floor Dysfunction: While the pelvic floor muscles themselves may not be directly affected by brachytherapy, the changes to urinary and sexual function may require pelvic floor rehabilitation to improve control and restore function.
The Role of Pelvic Floor Physiotherapy After Prostate Cancer Treatment
Pelvic floor physiotherapy is a specialized form of physical therapy designed to restore pelvic muscle function, alleviate pain, and address symptoms related to pelvic floor dysfunction. After prostate cancer treatments, pelvic floor physiotherapy can be a key component of recovery and rehabilitation. Here’s how pelvic floor physiotherapy can help:
Pelvic Floor Muscle Strengthening: One of the most common goals of pelvic floor physiotherapy is to strengthen weakened muscles. A physiotherapist will guide you through exercises that target the pelvic floor muscles to improve strength, reduce incontinence, and support sexual health.
Urinary Incontinence Management: Pelvic floor therapy helps restore bladder control by teaching exercises and techniques to strengthen the pelvic floor muscles. Patients may also be taught bladder training strategies and techniques for improving urinary retention.
Sexual Rehabilitation: Pelvic floor physiotherapy can help improve erectile function and address any sexual difficulties caused by prostate cancer treatments. Specialized exercises, including Kegel exercises, can help restore sexual function and improve pelvic health.
Pain Relief: If you experience discomfort or pain in the pelvic area after treatment, pelvic floor physiotherapy can help relieve tension and reduce pain. Manual therapy techniques can be used to release muscle tightness and improve blood flow to the affected areas.
Education and Lifestyle Modifications: Pelvic floor physiotherapists provide valuable education on managing symptoms and making lifestyle changes to support recovery. This includes posture correction, movement retraining, and strategies for managing pain or incontinence.
Conclusion
Prostate cancer treatments, such as surgery, radiation, and hormone therapy, can have a significant impact on pelvic floor health. The side effects of these treatments, including urinary incontinence, erectile dysfunction, and pelvic floor muscle weakness, can be challenging to manage. However, pelvic floor physiotherapy offers a non-invasive, effective approach to improving pelvic health, managing symptoms, and enhancing quality of life after prostate cancer treatment. If you are undergoing prostate cancer treatment or have experienced side effects, consulting with a pelvic floor physiotherapist can help you navigate recovery and restore your pelvic function.