How the brain and pelvic floor can work together
Introduction
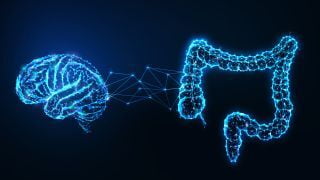
The human body is a remarkable and intricately interconnected system where various organs and systems communicate and influence each other. One such crucial connection is the gut-brain axis, which involves bidirectional communication between the gastrointestinal (GI) tract, commonly known as the gut, and the central nervous system (CNS), which comprises the brain and spinal cord. The gut-brain axis plays a significant role in regulating numerous physiological functions, including digestion, mood regulation, and even the health of the pelvic floor. In this article, we will delve into the concept of the gut-brain axis, its key components, and explore how it impacts the pelvic floor.
Understanding the Gut-Brain Axis:
The gut-brain axis refers to the complex network of bidirectional communication between the gut and the brain. It encompasses multiple components, including the enteric nervous system (ENS), the autonomic nervous system (ANS), the hypothalamic-pituitary-adrenal (HPA) axis, as well as various neurotransmitters, hormones, and immune cells.
- Enteric Nervous System (ENS):
The enteric nervous system, often referred to as the "second brain," is a sophisticated network of neurons embedded within the walls of the gastrointestinal tract. It is capable of functioning independently of the central nervous system (CNS) but also communicates with the brain. The ENS regulates various aspects of gut function, including motility (movement of food through the digestive tract), secretion of digestive enzymes and hormones, and local blood flow within the gut. Additionally, it plays a crucial role in modulating inflammation and the immune response within the gut.
2. Autonomic Nervous System (ANS):
The autonomic nervous system consists of two primary branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). These branches are responsible for regulating involuntary functions of the body, including those of the GI tract and the pelvic floor.
a) Sympathetic Nervous System (SNS): The SNS is responsible for the body's "fight-or-flight" response, which prepares the body for stress or danger. It can influence gut motility, blood flow, and sphincter function, potentially impacting the pelvic floor. When the SNS is activated, it can lead to increased muscle tension in the pelvic floor, potentially contributing to conditions such as pelvic pain and muscle dysfunction.
b) Parasympathetic Nervous System (PNS): The PNS promotes the body's "rest-and-digest" response, which helps regulate normal gut function, including digestion and relaxation of the pelvic floor muscles. Activation of the PNS supports healthy pelvic floor function and helps maintain a relaxed state, reducing the risk of pelvic floor disorders.
c) Hypothalamic-Pituitary-Adrenal (HPA) Axis: The hypothalamic-pituitary-adrenal (HPA) axis is a complex hormonal system involving the hypothalamus, pituitary gland, and adrenal glands. It plays a vital role in regulating the body's response to stress. Activation of the HPA axis can impact gut function and may contribute to pelvic floor dysfunction under chronic stress conditions. The HPA axis releases cortisol, a stress hormone that can affect the motility and sensitivity of the gut, potentially leading to pelvic floor symptoms.
3. Neurotransmitters, Hormones, and Immune Cells:
Neurotransmitters are chemical messengers that facilitate communication between neurons in the nervous system. Several neurotransmitters play a role in gut-brain communication, including serotonin, dopamine, and gamma-aminobutyric acid (GABA). These neurotransmitters influence gut motility, inflammation, and pain perception, all of which can impact the health of the pelvic floor. Serotonin, often referred to as the "feel-good" neurotransmitter, is predominantly found in the gastrointestinal system. It plays a role in regulating gut motility, secretion, and sensitivity. Imbalances in serotonin levels have been associated with conditions such as irritable bowel syndrome (IBS), which can contribute to pelvic floor dysfunction. Dopamine is another neurotransmitter that plays a role in the gut-brain axis. It is involved in regulating gut motility and can influence the function of the pelvic floor. Alterations in dopamine levels have been linked to gastrointestinal disorders, such as constipation or diarrhea, which can impact pelvic floor function.
GABA, an inhibitory neurotransmitter, helps regulate the excitability of neurons in the gut. It promotes relaxation and can have a calming effect on the gut and pelvic floor muscles. Dysfunction in GABA signaling has been associated with conditions like visceral hypersensitivity and pelvic pain.
Hormones also play a crucial role in gut-brain communication and can impact the health of the pelvic floor. Estrogen and progesterone, for instance, fluctuate during the menstrual cycle and menopause. These hormonal changes can influence gut motility, sensitivity, and pelvic floor function. Decreased levels of estrogen during menopause, for example, can contribute to changes in the vaginal and pelvic floor tissues, leading to symptoms such as vaginal dryness, urinary incontinence, and pelvic organ prolapse.
Immune cells, specifically those within the gut, also contribute to the gut-brain axis. Inflammatory molecules released by immune cells can affect gut function and subsequently impact the pelvic floor. Chronic inflammation in the gut, such as in conditions like inflammatory bowel disease (IBD), has been associated with an increased risk of pelvic floor dysfunction, including pelvic pain and bowel disturbances.
Impact of the Gut-Brain Axis on the Pelvic Floor:
The gut-brain axis exerts a significant influence on the health and function of the pelvic floor. Here are some key ways in which the gut-brain connection impacts the pelvic floor:
- Digestive Function and Bowel Movements:
The gut-brain axis plays a crucial role in regulating digestion and bowel movements. Communication between the gut and the brain ensures the coordinated movement of food through the digestive tract. Imbalances or disruptions in this communication can lead to conditions such as constipation or diarrhea, which can contribute to pelvic floor dysfunction, including pelvic pain and muscle tension.
2. Sensitivity and Pain Perception:
The gut-brain axis also influences the sensitivity and perception of pain in the pelvic region. When the gut is inflamed or irritated, it can send signals to the brain that can result in increased pain sensitivity, including pelvic pain. Similarly, chronic pain conditions in the pelvic region can also impact the gut-brain axis and contribute to gastrointestinal symptoms, such as changes in bowel habits or abdominal discomfort.
3. Emotional Well-being and Stress:
The gut-brain axis is intimately connected to emotions and stress responses. Stress, anxiety, and depression can disrupt the balance of gut bacteria, affect gut motility, and alter the production of neurotransmitters involved in gut-brain communication. These changes can impact the pelvic floor, leading to symptoms such as increased muscle tension, pelvic pain, and sexual dysfunction.
4. Hormonal Changes:
Hormonal fluctuations, particularly during menstrual cycles and menopause, can affect the gut-brain axis and subsequently impact the pelvic floor. Decreased estrogen levels during menopause, for example, can contribute to changes in the pelvic floor tissues, leading to symptoms such as vaginal dryness, urinary incontinence, and pelvic organ prolapse.
How Pelvic Physiotherapy Can Help:
Pelvic physiotherapy is a specialized form of physical therapy that focuses on the muscles, ligaments, and connective tissues of the pelvic floor. It aims to improve pelvic floor muscle function, restore balance, and alleviate symptoms associated with pelvic floor dysfunction. In the context of the gut-brain axis, pelvic physiotherapy can play a vital role in addressing pelvic floor issues influenced by the gut-brain connection. Here's how pelvic physiotherapy can help:
- Pelvic Floor Muscle Training:
Pelvic physiotherapy often involves pelvic floor muscle training, which includes exercises to strengthen and relax the pelvic floor muscles. By improving the coordination and strength of these muscles, pelvic physiotherapy can help address pelvic floor dysfunctions such as urinary incontinence, fecal incontinence, and pelvic organ prolapse. The training also includes teaching individuals to become more aware of their pelvic floor muscles, promoting a better mind-body connection.
2. Relaxation Techniques:
In addition to strengthening exercises, pelvic physiotherapy can incorporate relaxation techniques to help release tension in the pelvic floor muscles. These techniques may involve diaphragmatic breathing, which promotes relaxation of the pelvic floor and activates the parasympathetic nervous system, leading to a decrease in muscle tension. By addressing muscle tension and promoting relaxation, pelvic physiotherapy can contribute to reducing pelvic pain and improving overall pelvic floor function.
3. Education and Lifestyle Modifications:
Pelvic physiotherapists often provide education on proper bowel habits, bladder management, and dietary modifications to promote optimal gut health. They may offer guidance on optimizing hydration, fiber intake, and the importance of regular bowel movements to maintain a healthy gut-brain axis. Additionally, they can address any lifestyle factors that may contribute to pelvic floor dysfunction, such as excessive straining during bowel movements or poor posture, and provide strategies to manage and improve these aspects.
4. Manual Therapy Techniques:
Pelvic physiotherapy may involve manual therapy techniques, including internal and external myofascial release and trigger point therapy. These techniques aim to release tension, reduce muscle knots, and improve blood flow in the pelvic floor muscles. Manual therapy can be especially beneficial for individuals with pelvic pain syndromes or hypertonic pelvic floor muscles resulting from the impact of the gut-brain axis. By addressing muscle imbalances and trigger points, manual therapy can help alleviate pain and restore normal pelvic floor function.
5. Biofeedback:
Biofeedback is a commonly used tool in pelvic physiotherapy that provides real-time information on muscle activity and helps individuals gain awareness and control over their pelvic floor muscles. It can be particularly useful in cases of pelvic floor dysfunction influenced by the gut-brain axis. By visualizing muscle activity on a screen or through auditory cues, biofeedback helps individuals understand and modify their pelvic floor muscle function, enhancing coordination, relaxation, and strength.
Conclusion:
The gut-brain axis is a complex communication network that significantly influences the health and function of the pelvic floor. Understanding the connection between the gut, the brain, and the pelvic floor is essential for effectively addressing pelvic floor dysfunctions and related symptoms. Pelvic physiotherapy plays a crucial role in this process by focusing on improving pelvic floor muscle function, promoting relaxation, addressing muscle imbalances, and providing education on gut health. By addressing the impact of the gut-brain axis, pelvic physiotherapy offers a holistic approach to managing pelvic floor dysfunction and improving overall well-being. Consult with a qualified pelvic physiotherapist to determine the most appropriate treatment plan tailored to your specific needs.