Understanding the Link Between Them
Understanding the Link Between Them
Pelvic floor dysfunction and sacroiliac joint (SI joint) pain are two common issues that can profoundly impact a person’s daily life. While they may seem unrelated at first glance, these conditions are often intricately connected. Understanding the link between pelvic floor dysfunction and sacroiliac joint pain can help individuals manage both conditions more effectively and improve their overall quality of life.
What Is Pelvic Floor Dysfunction?
The pelvic floor is a group of muscles, ligaments, and connective tissues that form a supportive "hammock" at the base of the pelvis. These muscles provide support for vital organs such as the bladder, uterus, prostate, rectum, and small intestines, playing an essential role in functions like urination, bowel movements, and sexual activity.
Pelvic floor dysfunction (PFD) occurs when these muscles become either too tight or too weak to perform their normal functions. Symptoms of PFD can include urinary incontinence, pelvic pain, constipation, painful intercourse, and, in some cases, pelvic organ prolapse.
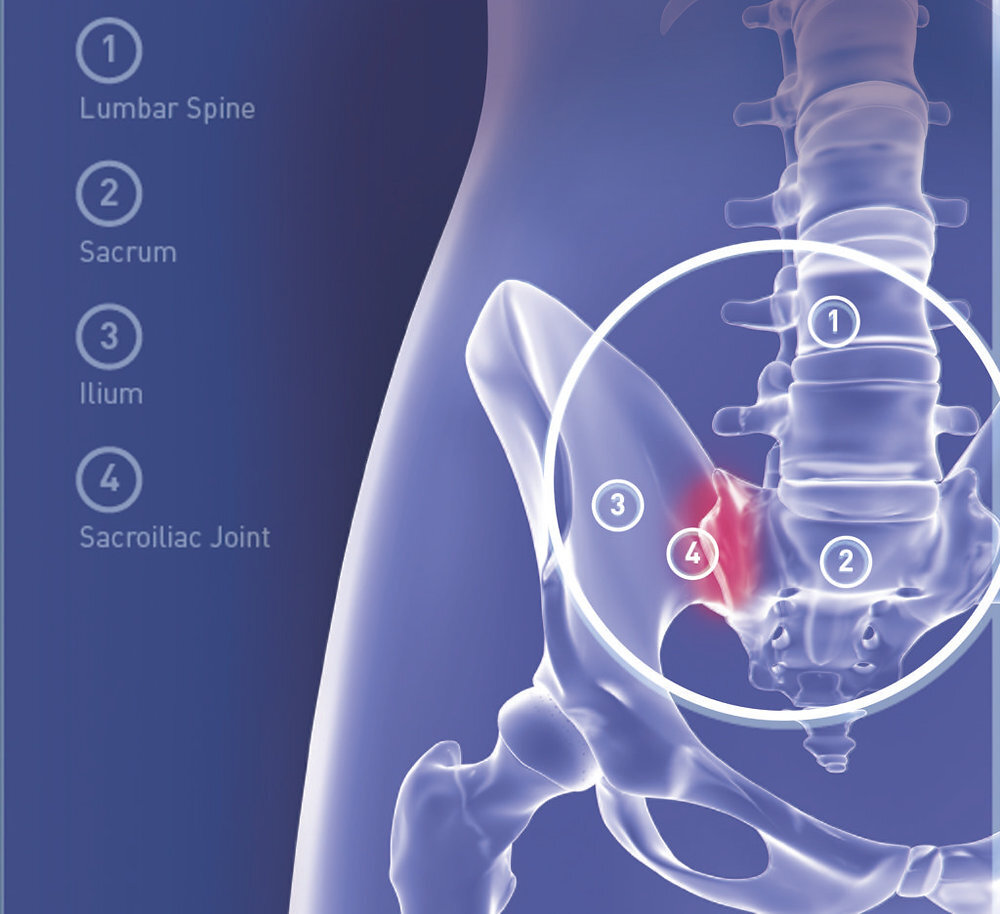
What Is Sacroiliac Joint Pain?
The sacroiliac (SI) joints are located where the sacrum (the triangular bone at the base of the spine) meets the iliac bones of the pelvis. These joints are crucial for transferring forces between the spine and the legs. They help with stability during activities like walking, running, and climbing stairs.
Sacroiliac joint pain (or sacroiliitis) arises when these joints experience inflammation or dysfunction, which can cause pain in the lower back, buttocks, and hips, potentially radiating down the legs. This pain can result from trauma, pregnancy, arthritis, or muscle imbalances that affect the way forces are transmitted through the pelvis.
The Link Between Pelvic Floor Dysfunction and SI Joint Pain
While pelvic floor dysfunction and sacroiliac joint pain affect different structures, they are closely linked through muscle imbalances and central sensitization. These factors can lead to increased pain and dysfunction in both areas, making it crucial to address both simultaneously.
- Muscle Imbalances and Pelvic Floor Dysfunction
Muscle imbalances in the pelvis are one of the primary ways that pelvic floor dysfunction and SI joint pain are connected. When the pelvic floor muscles are either too tight or too weak, they can impact the way the pelvis functions as a whole. These imbalances can affect the stability of the SI joints, even though the joints themselves do not have a large range of motion.
For example, tight pelvic floor muscles (a condition known as pelvic floor overactivity) can create abnormal tension in the pelvis. This increased muscle tension can affect the surrounding structures, including the SI joints, causing discomfort and even pain in the lower back and hips. On the other hand, weak pelvic floor muscles may fail to provide adequate support, leading to instability in the pelvis and contributing to SI joint pain.
These imbalances do not just affect the pelvic floor and SI joints directly. They can alter how the muscles of the hips, lower back, and abdomen function, creating a cycle of discomfort that impacts multiple areas of the body.
- Compensatory Movement Patterns
When the pelvic floor and SI joints are not functioning optimally, individuals often develop compensatory movement patterns to avoid pain or discomfort. For example, someone with pelvic floor dysfunction might unknowingly shift their posture or adopt abnormal movement strategies to relieve pelvic pressure. This can lead to altered mechanics in the pelvis and the SI joints, causing increased strain on the surrounding muscles.
In these cases, the body tries to protect itself from pain by “shifting” the load to other structures. This can create a vicious cycle of discomfort, as the altered movement patterns place additional stress on the SI joints, exacerbating the underlying dysfunction in the pelvic floor.
- The Role of Central Sensitization in Chronic Pain
Both pelvic floor dysfunction and sacroiliac joint pain can lead to central sensitization, a phenomenon in which the nervous system becomes hypersensitive to pain signals. In people with chronic pelvic or SI joint pain, the nervous system becomes more reactive, amplifying pain perception, even from non-painful stimuli.
For example, the muscles and tissues around the pelvic floor and SI joints may send pain signals to the brain due to muscle tension, inflammation, or abnormal movement patterns. Over time, this can lead to an increased sensitivity to pain. As a result, even slight movements or activities that wouldn’t normally cause discomfort might become painful, making it more difficult for individuals to recover and manage their pain effectively.
Central sensitization complicates treatment and recovery because it amplifies the pain, making it harder for people to perform necessary exercises or engage in rehabilitation. This is why addressing the central nervous system’s response to pain is just as important as addressing the physical issues of muscle imbalances and joint dysfunction.
Treatment and Management
To effectively treat both pelvic floor dysfunction and sacroiliac joint pain, a comprehensive approach is required. Treatment focuses on addressing the underlying muscle imbalances, reducing pain amplification through central sensitization, and restoring normal movement patterns.
- Pelvic Floor Rehabilitation
Pelvic floor physiotherapy is key in addressing issues related to muscle tightness, weakness, and imbalances. A pelvic floor therapist can teach exercises to both strengthen and relax the pelvic floor muscles. Proper muscle activation and relaxation techniques help restore balance in the pelvis, which can reduce stress on the SI joints and alleviate pain.
- Core and Hip Strengthening
Strengthening the muscles of the core, hips, and lower back can provide better stability for both the pelvic floor and the SI joints. Targeted exercises that improve the function of these muscle groups can help prevent compensatory movement patterns and reduce strain on the SI joints. Strengthening these areas also helps support the pelvic floor muscles, contributing to overall pelvic stability.
- Managing Central Sensitization
To address central sensitization, a combination of pain management techniques, such as desensitization exercises, gentle stretching, and stress-reducing activities (like mindfulness or deep breathing exercises), can help calm the nervous system and reduce pain amplification. Gradual desensitization exercises can help the body become less reactive to pain signals and increase tolerance to movement.
- Manual Therapy and Soft Tissue Work
Manual therapy, including techniques like myofascial release or trigger point therapy, can be used to reduce muscle tightness in the pelvic floor and surrounding areas. Soft tissue work can alleviate tension in the muscles and connective tissues, promoting greater flexibility and reducing pain.
Conclusion
Pelvic floor dysfunction and sacroiliac joint pain are often intertwined, with muscle imbalances and central sensitization contributing to the symptoms of both conditions. A comprehensive treatment plan that addresses these factors—through pelvic floor rehabilitation, core strengthening, pain management, and manual therapy—can help break the cycle of discomfort and improve overall pelvic health. If you are experiencing these issues, seeking help from a healthcare provider specializing in pelvic health is essential to finding a solution tailored to your needs.